In its August 2018 cybersecurity newsletter, the Department of Health and Human Services’ Office for Civil Rights has reminded HIPAA-covered entities of the importance of implementing physical, technical, and administrative safeguards to ensure the confidentiality, integrity, and availability of electronic protected health information (ePHI) that is processed, transmitted, or stored on electronic media and devices.
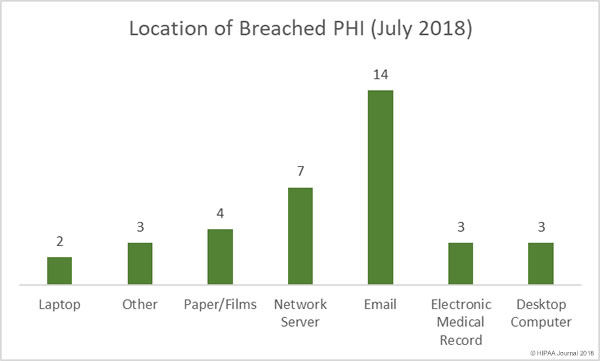
Electronic devices such as desktop computers, laptops, servers, smartphones, and tablets play a vital role in the healthcare, as do electronic media such as hard drives, zip drives, tapes, memory cards, and CDs/DVDs. However, the portability of many of those devices/media means they can easily be misplaced, lost, or stolen.
Physical controls are therefore essential. Anyone with physical access to electronic devices or media, whether healthcare employees or malicious actors, potentially have the ability to view, change, or delete data. Device configurations could be altered or malicious software such as ransomware or malware could be installed. All of these actions jeopardize the confidentiality, integrity, or availability of ePHI.
HIPAA – 45 CFR § 164.310(a)(1) – requires covered entities and their business associates to implement policies and procedures to restrict access to electronic devices and media and the facilities in which they are housed. 45 CFR § 164.310(d)(1) of the HIPAA Security Rule requires policies and procedures to be implemented to govern the receipt and removal of those devices into and out of an organization’s facility, as well as movement within the facility. Robust policies and procedures must be developed to ensure ePHI is appropriately protected at all times.
When developing policies and procedures covering portable electronic devices and media, OCR recommends that HIPAA covered entities and their business associates consider the following questions:
- Are records tracking the location, movements, alterations, repairs, and disposition of devices and media in place covering the entire life cycle of the devices/media?
- Does the organization’s record of device and media movement include the individual(s) responsible for such devices and media?
- Have members of the workforce (including management) received training on the correct handling of devices/media to ensure ePHI is safeguarded at all times?
- Have appropriate technical controls been implemented to ensure the confidentiality, integrity, and availability of ePHI, such as encryption, access controls and audit controls?
There are several methods for tracking electronic devices and media. Smaller healthcare organizations that only use a limited number of devices/media may be able to manually track the movement of their devices/media, although this becomes a major challenge if large numbers of devices are in use. In such cases, specialized inventory management software and databases may be more appropriate. OCR suggests the use of a bar-code system or RFID tags may make it easier to organize, identify, and track the movement of devices and media.
When deciding on the most appropriate device and media controls to implement, healthcare organizations and their business associates should be guided by their risk analysis and risk management processes. Full consideration should be given to size, complexity and capabilities; hardware and software capabilities; technical infrastructure; the cost of implementing security measures; and the probability and criticality of potential risks to ePHI.
Policies and procedures must also be developed and implemented to ensure that when devices/media reach end of life, all ePHI stored on the devices is permanently erased to prevent the information from being retrieved or reconstructed. OCR covered the secure disposal of ePHI in its July 2018 cybersecurity newsletter.
Organizations that fail to track electronic devices and media and ensure that ePHI is appropriately protected at all times run the risk of HIPAA fines for non-compliance.
The most recent example is University of Texas MD Anderson Cancer Center’s failure to encrypt ePHI on portable electronic devices. That violation resulted in a civil monetary penalty of $4,348,000.
The August 2018 cybersecurity newsletter can be downloaded on this link (PDF – 140KB)
The post Healthcare Organizations Reminded of Importance of Securing Electronic Media and Devices Containing ePHI appeared first on HIPAA Journal.